Atherosclerosis home=>news=>atherosclerosis=>general
(affects Type 1 AND Type 2 Diabetics)
General
Treatment
Pathophysiology
 |
Mortality and
Cardiovascular Events Increased in Non-diabetic Subjects
with Metabolic Syndrome; Fasting Glucose a Strong
predictor of Increased Mortality: A PreCIS Database
Cohort Study ADA 67th Annual Meeting Year: 2007
Abstract Number: 0975-P
Authors:KRUPA B. DOSHI, DANIELLE M.
BRENNAN, BRIAN M. HOAR, BYRON J. HOOGWERF, LESLIE CHO,
SANGEETA R. KASHYAP, Cleveland, OH
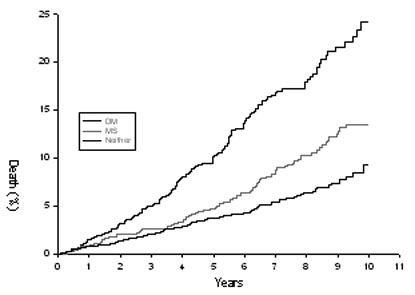
Results:We assessed cardiovascular (CV) risk, events and
mortality in non-diabetic subjects who met NCEP ATP III
criteria for Metabolic Syndrome (MS). We retrospectively
compared 1189 diabetics (DM) (age 59 [plusmn] 12 y, 65%
M, BMI 32 [plusmn] 7, FPG 150[plusmn] 58 mg/dL, HbA1c
7.6[plusmn] 1.8), 1241 MS ([gt] 3 components
NCEP-ATP III criteria) (55 [plusmn] 12y, 64% M, BMI 32
[plusmn] 5, FPG 93 [plusmn]14 mg/dL) and 3023
non-Metabolic Syndrome subjects ([lt] 3 components
NCEP-ATP III criteria) (C) (54 [plusmn] 14 y, 61% M, BMI
27 [plusmn] 5, FPG 85 [plusmn] 12 mg/dL) subjects who
presented to Preventive Cardiology clinic between
1995-2006. Initial blood work was done within 30 days of
first visit. The association with mortality was analyzed
with Cox proportional hazards model. The proportional
risk of mortality is represented with Kaplan-Meier
survival curves.
DM group has greatest mortality (fig.) and CV events (MI
30%, CHF 14%) vs. MS (24%, 5%) and C (18%, 3%) groups
(all P [lt] 0.001). Compared to C, MS subjects had
markedly increased mortality (fig.), CV events (MI, CHF)
and markedly atherogenic lipid profile [MS- (HDL 39
[plusmn] 10, Apo A 129 [plusmn] 26, Apo B 128 [plusmn]
37, CRP 5.5 [plusmn] 10.4, homocysteine 12.3 [plusmn]
4.4) mg/dL, ApoB/ApoA 1.02 [plusmn] 0.3] [C- (HDL 53
[plusmn] 17, Apo A 139 [plusmn] 31, Apo B 116 [plusmn]
35, CRP 4.1 [plusmn] 8.1, homocysteine 11.7 [plusmn] 4.5)
mg/dL, ApoB/ApoA 0.87 [plusmn] 0.4] (all P [lt]0.001
vs.C). In the multivariate cox proportional hazard model,
adjusting for age, gender, total cholestrol, fibrinogen,
Framingham scores, fasting glucose markedly increased C
index from 0.757 to 0.779 over other components of MS. In
summary, patients who meet the NCEP ATP III MS criteria
are at increased risk for mortality and CV events
compared to patients without MS. Fasting plasma glucose
is an important component of MS criteria that strongly
predicts death in this group.
[figure1]
Images:
Predictive
value of admission hyperglycaemia on mortality in
patients with acute myocardial infarction (Diabet. Med. [2006] 23:1370–1376)
Abstract
Rationale and aim In patients with an acute myocardial
infarction, admission hyperglycaemia (AH) is a major risk
factor for mortality. However, the predictive value of
AH, when the risk score and use of guidelines-recommended
treatments are considered, is poorly documented.
Methods The first fasting plasma glucose levels after
admission, risk level, guidelines-recommended treatment
use and 1-year mortality were recorded. Patients with
first fasting glucose level after admission > 7.7
mmo/l were considered to have AH. Results Three
hundred and twenty patients with ST segment elevation
myocardial infarction (STEMI) and 404 with non-ST segment
elevation myocardial infarction (NSTEMI) were included.
One hundred and seventy-five (24%) patients had
pre-existing diabetes (diabetes group), 154 (21%) had AH
(AH+ group) and the remainding 395 (55%) had neither
diabetes nor AH (AH– group). The Global Registry of
Acute Coronary Events (GRACE) risk score was lower in the
AH– group, but the use of guidelines-recommended
treatment was comparable in all groups. At 1 year, the
mortality rate was higher in the AH+ group compared with
the AH– group (18.8 vs. 6.1%, P < 0.01) and
similar to that in the diabetes group (18.8 vs. 16.6%, P
= NS). The relation between glycaemic status and
mortality remained strong [AH+ vs. AH–, OR = 3.0
(1.5, 6.0) and diabetes vs. AH–, OR = 3.6 (1.7,
6.6)] after adjustment for the GRACE risk score [OR = 2.4
(1.8, 3.1) per 10% increase] and for treatment score [OR
= 0.7 (0.6, 0.8) per 10% increase].Conclusions
In patients without a history of diabetes, the presence
of AH indicates an increased risk of 1-year mortality,
similar to that of patients with diabetes, even when the
risk score and use of guidelines-recommended treatment
are controlled for. Keywords:-ACE,
angiotensin converting enzyme; AH, admission
hyperglycaemia; GRACE, Global Registry of Acute Coronary
Events; MI, myocardial infarction; NSTEMI, non-ST segment
elevation MI; STEMI, ST elevation MI stress
hyperglycaemia, diabetes, myocardial infarction, risk
score
Study Putatively Showing Excess CV Mortality among Hospitalized US Blacks Fails to Correct for Either Newness or Degree of Diabetes (Circulation [2005] 112:2634-2641) Background— African Americans are more likely to be seen by physicians with less clinical training or to be treated at hospitals with longer average times to acute reperfusion therapies. Less is known about differences in health outcomes. This report compares risk-adjusted mortality after acute myocardial infarction (AMI) between US hospitals with high and low fractions of elderly black AMI patients. Methods and Results— A prospective cohort study was performed for fee-for-service Medicare patients hospitalized for AMI during 1997 to 2001 (n=1 136 736). Hospitals (n=4289) were classified into approximate deciles depending on the extent to which the hospital served the black population. Decile 1 (12.5% of AMI patients) included hospitals without any black AMI admissions during 1997 to 2001. Decile 10 (10% of AMI patients) included hospitals with the highest fraction of black AMI patients (33.6%). The main outcome measures were 90-day and 30-day mortality after AMI. Patients admitted to hospitals disproportionately serving blacks experienced no greater level of morbidities or severity of the infarction, yet hospitals in decile 10 experienced a risk-adjusted 90-day mortality rate of 23.7% (95% CI 23.2% to 24.2%) compared with 20.1% (95% CI 19.7% to 20.4%) in decile 1 hospitals. Differences in outcomes between hospitals were not explained by income, hospital ownership status, hospital volume, census region, urban status, or hospital surgical treatment intensity. Conclusions— Risk-adjusted mortality after AMI is significantly higher in US hospitals that disproportionately serve blacks. A reduction in overall mortality at these hospitals could dramatically reduce black-white disparities in healthcare outcomes. Key Words: death, sudden • myocardial infarction • hospitals • outcomes • race
Abnormal fasting plasma glucose - high and low - linked with ischemic stroke (Stroke [2004] 35: 2351-2355) Background and Purpose— Diabetes and impaired fasting glucose are diagnosed based on an elevated plasma glucose level after an overnight fast. The diagnostic cutpoint of diabetes arises from the threshold for development of microvascular complications. Our aim was to examine the associations between clinical relevant categories of fasting glucose levels and the risk of incident ischemic stroke. Methods— Patients with documented coronary heart disease who were screened for inclusion in a secondary prevention clinical trial (n=13 999) were followed-up. At baseline, medical histories were obtained and plasma glucose and lipids assessed at a central study laboratory. During a 6- to 8-year follow-up period 1037 cases were identified with ischemic cerebrovascular disease, of which, after reviewing hospital records with diagnoses of cerebrovascular disease, 576 cases were verified to have had ischemic stroke or transient ischemic attacks. Results— Increasing fasting glucose level categories were positively associated with increasing age, male gender, body mass index, hypertension, total cholesterol, and triglycerides, and were inversely associated with high-density lipoprotein cholesterol and percent high-density lipoprotein of total cholesterol. In comparison with patients with fasting glucose levels of 90 to 99 mg/dL (n=3706) who constitute the largest category, the odds ratios of ischemic cerebrovascular disease, adjusting for potential confounders, were 1.47 (95% CI, 1.07 to 2.02) for fasting glucose <80, 1.22 (0.98 to 1.52) for 80 to 89, 1.27 (1.02 to 1.60) for 100 to 109, 1.60 (1.26 to 2.03) for 110 to 125, 1.82 (1.33 to 2.49) for 126 to 140, and 2.82 (2.32 to 3.43) for >140 mg/dL. Similar J-shaped associations were observed in analysis excluding patients with known diagnosis of diabetes mellitus. Conclusions— The association between fasting plasma glucose and incident ischemic cerebrovascular events in patients with pre-existing atherothrombotic disease is J-shaped. Rates increase for fasting plasma glucose levels >100 mg/dL and also for those with low fasting glucose levels. These findings may carry important implications for prevention strategies.
Sulfonylureas attenuate electrocardiographic ST-segment elevation during an acute myocardial infarction in diabetics.OBJECTIVES: The aim of this study was to determine whether sulfonylureas attenuate ST-segment elevation in diabetics during acute myocardial infarction (AMI). BACKGROUND: Sulfonylureas block adenosine triphosphate-sensitive potassium channels found in the pancreas and heart. Animal studies have demonstrated that opening of these cardiac channels results in ST-segment elevation during AMI, and pretreatment with sulfonylureas blunts these ST-segment changes. METHODS: We performed a retrospective study of diabetic patients hospitalized with AMI over a four-year period in Framingham, Massachusetts. Electrocardiograms obtained on arrival were analyzed for standard ST-segment criteria for thrombolytic therapy (>1 mm in two or more contiguous leads). Results were compared between the study group (40 patients taking sulfonylureas) and control group (48 patients taking alternative hypoglycemic agent). RESULTS: Demographics were similar for both groups apart from a female preponderance in the study group. A significantly higher percentage of patients in the study group did not meet ST-segment criteria for thrombolytic therapy as compared with the control group (53% vs. 29%, p = 0.02). This difference was most prominent in patients with peak creatinine phosphokinase levels between 500 and 1,000 mg/dl (86% vs. 22%, p = 0.04). The magnitude of ST-segment elevation and the frequency of thrombolytic therapy were significantly lower in the sulfonylurea group than in the control group (1.1 +/- 1.0 mm vs. 2.1 +/- 2.7 mm, p = 0.02 and 20% vs. 40%, p = 0.04, respectively). CONCLUSIONS: Sulfonylurea therapy appears to attenuate the magnitude of ST-segment elevation during an AMI, resulting in failure to meet criteria for thrombolytic therapy and as a consequence leading to inappropriate withholding therapy in this subset of diabetic patients. (J Am Coll Cardiol. [2003]17;42(6):1017-21.PMID: 13678923)
Type 2 diabetic patients found to have incidental carotid bruits have >6 times the risk of first stroke in the first 2 years than patients without a bruit (Stroke [2003]34:2145) Background and Purpose— We sought to examine prospectively the relationship between asymptomatic carotid bruit and stroke in type 2 diabetes. Methods— We studied 1181 (91.3%) of a community-based sample of 1294 patients with type 2 diabetes. These patients had no history of cerebrovascular disease at recruitment during 1993–1996 and were followed until the end of January 2002. Hospital morbidity and death register data relating to cerebrovascular events were also available. Cox proportional hazards models were used to determine whether carotid bruit status was an independent predictor of stroke and to identify other significant cerebrovascular risk factors. Results— One hundred thirty-four patients (11.3%) suffered a first stroke during 6.5ą2.2 (meanąSD) years of follow-up. In the first 2 years after study entry, first stroke (n=45/1181; 3.8%) was strongly predicted by the presence of carotid bruit(s) after adjustment for known cardiovascular risk factors and other potentially confounding variables (hazard ratio, 6.7; 95% CI, 3.0 to 14.9; P<0.001). Between 2 years and census, first stroke (n=89/1083; 8.2%) was not associated with carotid bruit(s) (P=0.97). Age and diastolic blood pressure were other determinants of stroke in the first 2 years, while age, atrial fibrillation/flutter, and microalbuminuria were independent predictors of subsequent stroke. Conclusions— Type 2 diabetic patients found to have incidental carotid bruits have >6 times the risk of first stroke in the first 2 years than patients without a bruit and should receive intensified management of vascular risk factors. Carotid imaging with a view to surgical intervention in these patients remains controversial. Key Words: carotid artery diseases • diabetes mellitus, non-insulin-dependent • stroke
MCP-1 is insulin-responsive and induces insulin resistance (Proc. Natl. Acad. Sci. USA, 10.1073/pnas.1133870100) This study identifies monocyte chemoattractant protein 1 (MCP-1) as an insulin-responsive gene. It also shows that insulin induces substantial expression and secretion of MCP-1 both in vitro in insulin-resistant (IR) 3T3-L1 adipocytes and in vivo in IR obese mice (ob/ob). Thus, MCP-1 resembles other previously described genes (e.g., PAI-1 and SREBP-1c) that remain sensitive to insulin in IR states. The hyperinsulinemia that frequently accompanies obesity and insulin resistance may therefore contribute to the altered expression of these and other genes in insulin target tissues. In vivo studies also demonstrate that MCP-1 is overexpressed in obese mice compared with their lean controls, and that white adipose tissue is a major source of MCP-1. The elevated MCP-1 may alter adipocyte function because addition of MCP-1 to differentiated adipocytes in vitro decreases insulin-stimulated glucose uptake and the expression of several adipogenic genes (LpL, adipsin, GLUT-4, aP2, beta3-adrenergic receptor, and peroxisome proliferator-activated receptor gamma). These results suggest that elevated MCP-1 may induce adipocyte dedifferentiation and contribute to pathologies associated with hyperinsulinemia and obesity, including type II diabetes.
In-hospital hyperglycemia represents an important marker of poor clinical outcome and mortality in patients with and without a history of diabetes. (JCEM [2002] 87:978-982) Admission hyperglycemia has been associated with increased hospital mortality in critically ill patients; however, it is not known whether hyperglycemia in patients admitted to general hospital wards is associated with poor outcome. The aim of this study was to determine the prevalence of in-hospital hyperglycemia and determine the survival and functional outcome of patients with hyperglycemia with and without a history of diabetes. We reviewed the medical records of 2030 consecutive adult patients admitted to Georgia Baptist Medical Center, a community teaching hospital in downtown Atlanta, GA, from July 1, 1998, to October 20, 1998. New hyperglycemia was defined as an admission or in-hospital fasting glucose level of 126 mg/dl (7 mmol/liter) or more or a random blood glucose level of 200 mg/dl (11.1 mmol/liter) or more on 2 or more determinations. Hyperglycemia was present in 38% of patients admitted to the hospital, of whom 26% had a known history of diabetes, and 12% had no history of diabetes before the admission. Newly discovered hyperglycemia was associated with higher in-hospital mortality rate (16%) compared with those patients with a prior history of diabetes (3%) and subjects with normoglycemia (1.7%; both P < 0.01). In addition, new hyperglycemic patients had a longer length of hospital stay, a higher admission rate to an intensive care unit, and were less likely to be discharged to home, frequently requiring transfer to a transitional care unit or nursing home facility.Our results indicate that in-hospital hyperglycemia is a common finding and represents an important marker of poor clinical outcome and mortality in patients with and without a history of diabetes. Patients with newly diagnosed hyperglycemia had a significantly higher mortality rate and a lower functional outcome than patients with a known history of diabetes or normoglycemia
CRP is a strong independent predictor of short and long-term mortality after non–ST-elevation acute coronary syndromes (NSTACS) that are treated with very early revascularization Circulation. [2002]105:1412.) Background— This study sought to evaluate the predictive value of C-reactive protein (CRP) on long-term mortality in non–ST-elevation acute coronary syndromes (NSTACS) that were treated with a very early aggressive revascularization strategy. Methods and Results— We conducted a prospective cohort study in 1042 consecutive patients with NSTACS who were undergoing coronary angiography and subsequent coronary stenting of the culprit lesion as the primary revascularization strategy within 24 hours. Levels of CRP were determined on admission. The patients were followed for a mean of 20 months. In-hospital mortality was significantly higher in patients with a CRP>10 mg/L (3.7% versus 1.2% with CRP<3 mg/L and versus 0.8% with CRP of 3 to 10 mg/L; relative risk for CRP>10 mg/L compared with CRP<=10 mg/L was 4.2, 95% confidence interval [CI] was 1.6 to 11.0; P=0.004). The increase in mortality in patients with CRP>10 mg/L persisted during follow-up. Long-term mortality was 3.4% with CRP<3 mg/L, 4.4% with CRP between 3 and 10 mg/L, and 12.7% with CRP>10 mg/L (relative risk for CRP>10 mg/L compared with CRP<=10 mg/L, 0.8; 95% CI, 2.3 to 6.2; P<0.001). In addition, Kaplan-Meier survival analysis demonstrated a significantly reduced survival at 4 years in patients with a CRP>10 mg/L (78% versus 88% for a CRP of 3 to 10 mg/L and versus 92% for CRP<3 mg/L; P<0.001 by log-rank). In a multivariate analysis, CRP was an independent predictor of long-term mortality. Patients with a CRP>10 mg/L had >4 times the risk of death (odds ratio, 4.1; 95% CI, 2.3 to 7.2). Conclusion— CRP is a strong independent predictor of short and long-term mortality after NSTACS that are treated with very early revascularization.
NHLBI Issues NCEP iii Guidelines (15 May 2001)
AHA (American Heart Association)Recommendation
Diabetes
and Decline in Heart Disease Mortality
To the Editor: Dr Gu and colleagues1 found that patients with diabetes experienced fewer declines in heart disease mortality in 1982-1984 vs 1971-1975, compared with nondiabetic individuals during the same periods, and suggest that the incidence of coronary heart disease may have decreased less in patients with diabetes. However, since weight gain is a known complication of insulin and oral hypoglycemic agents, it is possible that weight gain and associated hyperlipidemia secondary to medical management is preventing individuals with type 2 diabetes from fully participating in the declining mortality from coronary heart disease.
John
M. Poothullil, MD
Brazosport Memorial Hospital
Lake Jackson, Tex
1. Gu K, Cowie CC, Harris MI.
Diabetes and decline in heart disease mortality in US
adults. JAMA. 1999;281:1291-1297. ABSTRACT | FULL TEXT | PDF | MEDLINE
![]()
In Reply: Undoubtedly, many factors influenced the lower decline in mortality from ischemic heart disease among patients with diabetes compared with nondiabetic patients during 1971 to 1993. The well-known mortality decline in the general population has been attributed to reduction in cardiovascular risk factors and better treatment of patients with heart disease.1 Given the lower declines in heart disease mortality for diabetic patients in our study, these changes appear to have been less favorable or less effective for people with diabetes. Obesity became much more prevalent during the period of our study and affected both diabetic and nondiabetic adults.
Numerous
mechanisms underlie the higher mortality of patients with
diabetes. Several lines of evidence suggest that more
aggressive management of coronary heart disease in these
patients would lower their increased mortality risk.
Patients with diabetes have a significant increase in
mortality within the first 30 days and in the first year
after myocardial infarction,2 and in operative
mortality after coronary artery bypass grafting.3 In certain patients,
percutaneous transluminal coronary angiography has a
higher mortality risk than coronary artery bypass
grafting.3 Angiotensin-converting
enzyme inhibitors, beta-blockers, and aspirin have been
shown to be more effective in diabetic than nondiabetic
patients.4, 5 The DIGAMI (Diabetes
Mellitus, Insulin Glucose Infusion in Acute Myocardial
Infarction) study showed that tight glucose control
reduces the risk of mortality in the first year and at
3.5 years after myocardial infarction in diabetic
patients.6 Thus, while there may be
other factors that contribute to increased mortality from
coronary heart disease in patients with diabetes, the
available data suggest that failure to apply proven
therapies may explain, at least in part, the trends noted
in mortality of patients with diabetes.
Maureen I. Harris, PhD, MPH
National Institutes of Health
Bethesda, Md
1. Hunink MG, Goldman L, Tosteson
AN, et al. The recent decline in mortality from coronary
heart disease, 1980-1990: the effect of secular trends in
risk factors and treatment. JAMA.
1997;277:535-542. MEDLINE
2. Miettinen H, Lehto S, Salomaa V,
et al. Impact of diabetes on mortality after the first
myocardial infarction. The FINMONICA Myocardial
Infarction Register Study Group. Diabetes Care.
1998;21:69-75. MEDLINE
3. Bypass Angioplasty
Revascularization Investigation (BARI) Investigators.
Comparison of coronary bypass surgery with angioplasty in
patients with multivessel disease. N Engl J Med.
1996;335:217-225.
4. Kjekshus J, Gilpin E, Cali C,
Blackney A, Henning H, Ross J. Diabetic patients and
beta-blockers after acute myocardial infarction. Eur
Heart J. 1990;11:43-50. MEDLINE
5. Zuanetti G, Latini R, Maggioni A,
Franzosi M, Santoro L, Tognoni G, for the GISSI-3
investigators. Effect of the ACE-inhibitor lisinopril on
mortality in diabetic patients with acute myocardial
infarction: data from the GISSI-3 study. Circulation.
1997;96:4239-4245. MEDLINE
6. Malmberg K. Prospective
randomized study of intensive insulin treatment on long
term survival after acute myocardial infarction in
patients with diabetes mellitus. BMJ.
1997;314:1512-1515. MEDLINE
Presence of more severe retinopathy or
visual impairment in diabetic patients is a risk
indicator for increased risk of ischemic heart disease
death. Presence of these ocular conditions may identify
individuals who should be under care for cardiovascular
disease.
The
greatest cost savings in diabetes care is to be had from
reducing cardiovascular complications
Silent
Myocardial Ischemia with significant lesions occurs in
20.9% of type 2 diabetic male patients who are totally
asymptomatic for CAD
A
Free Screening Being Offered nation-wide called Legs
for Life aims to screen tens of
thousands of people in hopes of raising awareness of peripheral
vascular disease - PVD - a potentially
fatal condition that millions of Americans have but don't
realize - which affects one in 20 people over 50 years
old. Smokers, the overweight, and people
with diabetes, high blood pressure and
high cholesterol are at increased risk.
Eight to 10 million people have the condition. One-third
of people who have PVD do not
experience any symptoms including, most commonly,
pain on walking.
The Legs for Life program is
sponsored in part by the Society of
Cardiovascular and Interventional Radiology (SCVIR).
People interested in learning more about PVD or in
locating a local screening site can visit the Legs for
Life Internet site at www.legsforlife.org or call the
SCVIR toll-free number, (877)
35SCVIR (877-357-2847).
New
Fronts in the War on Diabetes in Adults
Diabetes (1) predicts
and (2) correlates with index of *In-Stent Restenosis*
Reload The
National Diabetes Center Frames
Home Page